If you're looking for the best therapy for PTSD, the sheer number of options can feel overwhelming right from the start. But here's the key takeaway, backed by decades of research: the most effective treatments are trauma-focused therapies. This is a specific category of psychotherapy, and it's considered the gold standard for a reason—it directly addresses the traumatic memory to help your brain finally process what happened.
Finding What "Best" Means for Your Healing Journey
Starting the journey to recover from Post-Traumatic Stress Disorder means letting go of the idea that there's a single "best" therapy for everyone. The truth is, the most effective approach is the one that fits you—your specific experiences, your needs, and what you're comfortable with.
Think of it like choosing the right tool for a job. You wouldn't use a hammer to turn a screw. While several tools might get a job done, one is almost always better suited for the task. When it comes to PTSD, the evidence consistently points to therapies that don't just talk around the trauma but actually engage with it directly.
The Gold Standard: Trauma-Focused Care
This guide is designed to cut through the noise and focus on what both clinical research and real-world experience show works best. The most important thing to know is that trauma-focused psychotherapies deliver the most reliable and lasting results. These aren't just general "talk it out" sessions; they are highly structured methods designed to help you process traumatic memories so they no longer control your life.
The goal of effective PTSD treatment is to help your brain correctly file away the traumatic memory. Instead of feeling like a constant, present-day threat, it can finally become a part of your past. This is what stops the flashbacks, nightmares, and that feeling of always being on edge.
We’re going to walk through some of the most powerful, evidence-based options available. By the end, you'll have the knowledge you need to make a confident, informed decision and find a clear path forward.
Your Local Path to Healing in Arizona
For those in Arizona, getting this level of specialized care is more accessible than you might think. Here at reVIBE Mental Health, our teams are experts in proven treatments like EMDR and Trauma-Focused CBT. We're ready to help at our five convenient locations:
- Chandler: 3377 S Price Rd, Suite 105
- Phoenix Deer Valley: 2222 W Pinnacle Peak Rd, Suite 220
- Phoenix PV: 4646 E Greenway Road, Suite 100
- Scottsdale: 8700 E Via de Ventura, Suite 280
- Tempe: 3920 S Rural Rd, Suite 112
Taking that first step is simple. Just give us a call at (480) 674-9220.
How Trauma-Focused CBT Helps You Heal
Think of your brain's reaction to trauma like a well-worn, negative groove on a record. Every time something reminds you of the event, the needle jumps right back into that same distressing track, playing the same painful song of fear, anxiety, and distress.
Trauma-Focused Cognitive Behavioral Therapy (TF-CBT) is a hands-on, skills-based approach that helps you lift the needle and cut a new groove. It’s not about just talking about what happened; it's about actively changing your relationship with the traumatic memories so they no longer have control over your present.
TF-CBT isn't a single therapy but a family of highly effective, evidence-backed treatments for PTSD. Two of the most proven and widely used approaches are Prolonged Exposure (PE) and Cognitive Processing Therapy (CPT). They both lead to the same destination—healing—but they take slightly different roads to get there.
Prolonged Exposure (PE): Facing the Fear to Reclaim Your Life
It’s completely human to want to avoid things that remind you of a traumatic event. You might steer clear of certain places, shut down specific thoughts, or sidestep difficult conversations. But over time, this avoidance can make your world feel smaller and smaller, giving the trauma more and more power.
Prolonged Exposure (PE) is designed to gently but directly break this cycle of fear and avoidance.
The core principle behind it is habituation. Imagine dipping your toes into a cold lake. At first, the shock of the cold is intense. But the longer you stay in, the more your body adjusts until the temperature feels normal. PE applies this same idea to traumatic memories and triggers.
In the safety of a therapy session, you’ll work with your therapist to gradually face the things you’ve been avoiding. This happens in two key ways:
- Imaginal Exposure: You’ll talk through the traumatic memory in detail, out loud, several times. This might sound intimidating, but it's a crucial step in teaching your brain that the memory itself is just that—a memory. It's not happening now, and it can't hurt you.
- In Vivo Exposure: "In vivo" simply means "in real life." You and your therapist will create a list of safe places or situations you've been avoiding. Then, you'll start re-engaging with them, one step at a time, until they no longer trigger that overwhelming sense of dread.
The logic of PE is simple but profound: what you avoid, you fear. By safely and intentionally confronting the memories and situations you’ve been running from, you send a powerful new message to your brain: "The danger is over. I am safe now."
Cognitive Processing Therapy (CPT): Changing the Story the Trauma Wrote
Trauma does more than just create painful memories; it can fundamentally warp the way you see yourself, other people, and the world. Cognitive Processing Therapy (CPT) zeroes in on these distorted beliefs, which therapists call "stuck points."
Stuck points are the painful conclusions your brain drew in the aftermath of trauma. They often sound like this:
- "If I had done something different, it wouldn't have happened. It's my fault."
- "I can never trust anyone again."
- "The world is completely unsafe, and I'm powerless to protect myself."
- "I'm broken beyond repair."
CPT is a structured, 12-session therapy that empowers you to challenge these deeply ingrained beliefs. You’ll learn to act like a detective, examining the evidence for and against your stuck points. By questioning these automatic thoughts and exploring new perspectives, you can develop a more balanced and accurate way of thinking.
This process doesn't erase what happened, but it fundamentally changes the meaning you've attached to it. The trauma becomes an event that happened to you, not the defining story of who you are.
Because they are so structured and backed by decades of research, both PE and CPT are widely considered the gold standard for treating PTSD. Time and again, studies confirm their effectiveness. In fact, a deep dive into the data shows that psychotherapy approaches like these can have an impact more than double that of medication alone, leading to significantly higher recovery rates. You can explore the research yourself to learn more about these powerful findings.
Comparing Key TF-CBT Approaches for PTSD
Seeing these two powerful therapies side-by-side can make it easier to understand which one might be a better fit for you. While both are highly effective, they tackle the problem from different angles.
| Feature | Prolonged Exposure (PE) | Cognitive Processing Therapy (CPT) |
|---|---|---|
| Primary Focus | Reducing the physical fear response and avoidance behaviors tied to trauma reminders. | Changing the unhelpful beliefs ("stuck points") that the trauma created about yourself, others, and the world. |
| Key Method | Gradual and repeated exposure—first by recounting the memory (imaginal), then by facing avoided situations (in vivo). | Identifying, challenging, and reframing distorted thoughts and beliefs using structured worksheets and exercises. |
| Ideal For | People whose main symptoms are intense fear, panic attacks, and avoidance of specific triggers and situations. | People who struggle with powerful feelings of guilt, shame, self-blame, or a shattered sense of trust and safety. |
| Talking About Trauma | Involves retelling the traumatic event in detail to process the memory and neutralize its emotional power. | Can be done with or without a detailed account of the trauma itself; the main focus is on the thoughts about the event. |
Ultimately, the best choice depends on your unique symptoms and experiences, and it’s a decision you’ll make together with a qualified therapist. Understanding how each approach works is the first, most powerful step toward finding the right path for your healing journey.
How EMDR Helps Your Brain Reprocess Traumatic Memories
While some therapies focus on actively changing your thoughts and behaviors, another powerful approach works on a deeper, more subconscious level. What if you could help your brain properly file away traumatic memories so they no longer hijack your present? That’s the entire premise behind Eye Movement Desensitization and Reprocessing (EMDR).
Imagine a traumatic memory is like a computer file that crashed while saving. It’s corrupted, fragmented, and every time the system tries to access it, everything freezes up. The memory isn't properly stored; it’s stuck in your brain's active RAM, constantly interfering with your daily life.
EMDR therapy acts like a skilled IT specialist. It doesn't delete the file, but it runs a defrag process. It helps your brain's own information processing system access the corrupted file, repair it, and then store it correctly on the hard drive. The memory becomes part of your history, not a glitch that constantly crashes your system.
The Science of Bilateral Stimulation
So, how does this "re-filing" process actually work? The unique engine of EMDR is something called bilateral stimulation (BLS). This just means engaging both sides of the brain in a rhythmic, back-and-forth pattern. Most often, this is done by following your therapist's fingers with your eyes from side to side.
But BLS can also involve alternating tones you listen to in headphones or gentle taps on your hands or knees. The specific method doesn't matter as much as the rhythm.
This rhythmic stimulation is thought to activate the same systems in your brain that are at work during REM (rapid eye movement) sleep. That’s the stage of sleep where your brain naturally processes the day's events and consolidates memories. By kick-starting this process while you briefly hold a traumatic memory in mind, BLS seems to "unstick" the memory, allowing it to connect with more helpful information and lose its intense emotional charge.
This diagram shows the basic journey in most trauma-focused therapies—from identifying the "stuck points" to challenging them and, finally, rewiring your brain's response.
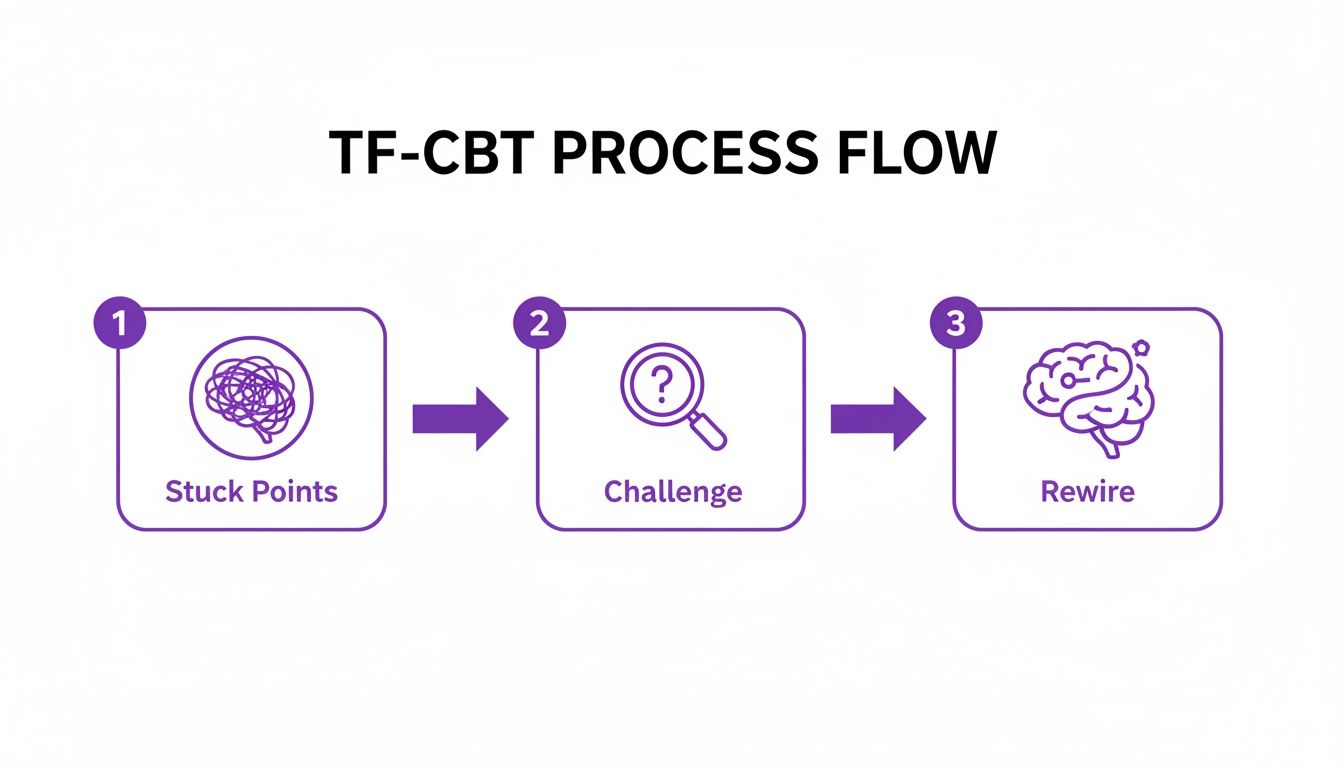
The goal is always to move from painful, automatic reactions to healthier, more intentional ones.
What to Expect During EMDR Sessions
EMDR isn't just waving fingers back and forth; it's a highly structured, eight-phase therapy. This organized approach makes sure you're prepared, feel safe, and are stable throughout the entire process.
Here’s a quick rundown of the phases:
- Phase 1: History and Treatment Planning: Your therapist gets a full picture of your background and helps you identify the specific memories or "targets" to work on.
- Phase 2: Preparation: This is crucial. You'll learn grounding techniques and coping skills to manage any tough emotions that come up. You are always in control.
- Phase 3: Assessment: For each target memory, you'll identify the associated image, a negative belief about yourself (e.g., "I'm not safe"), and where you feel it in your body.
- Phase 4: Desensitization: Here's where the bilateral stimulation begins. You’ll hold the memory in mind while doing the eye movements. The goal is simply to let your brain make new connections until the memory's disturbance level drops.
- Phase 5: Installation: Once the memory no longer feels upsetting, you'll work on strengthening a positive belief to replace the old negative one (e.g., "I can handle this").
- Phase 6: Body Scan: You'll scan your body for any lingering tension or discomfort related to the memory, ensuring it’s fully processed.
- Phase 7: Closure: Every session ends with you feeling grounded and calm, regardless of what came up.
- Phase 8: Re-evaluation: The next session starts by checking in on your progress to make sure the positive changes are sticking.
Perhaps the biggest draw for EMDR is that you don't have to talk about the traumatic event in exhaustive detail. For many people, this makes it an incredible option—especially when recounting the story feels impossible or re-traumatizing.
The therapy trusts your brain to do the healing work it’s designed to do. Your therapist is just a skilled and supportive guide for the journey.
To get a deeper look at this process, you can explore a detailed overview of EMDR therapy at reVIBE Mental Health. This treatment is available at our offices in Scottsdale, Chandler, Tempe, and Phoenix. Just give us a call at (480) 674-9220 to learn more.
Hitting PTSD From Both Sides: Why Therapy and Medication Work Better Together
For a lot of people navigating PTSD, recovery isn't a simple choice between therapy or medication. It's often about using both. Think of it this way: while powerful therapies like EMDR and Cognitive Processing Therapy (CPT) are designed to get to the root of the trauma, medication can be a critical partner in that journey. Combining them often builds the most solid foundation for getting your life back.
Imagine you've had a major injury. Therapy is the hard, focused physical rehab you need to do to actually heal the muscle and regain function. Medication is like the pain management that allows you to show up for your appointments and actually do the tough exercises without being completely overwhelmed. It makes the real work possible.
How Medication Gives Therapy a Boost
Medication doesn't "cure" PTSD. What it can do is manage the most intense, disruptive symptoms that make it feel impossible to even start the deep work therapy requires. When you're constantly on edge, drowning in anxiety, or so exhausted from insomnia that you can't think straight, engaging in therapy can feel like a monumental task.
That's where psychiatric medication comes in. It can create just enough stability and breathing room to let you fully show up and participate in your sessions.
- It turns down the "symptom volume," making it easier to focus and learn the new coping skills your therapist is teaching.
- It can improve your mood and sleep, giving you the basic mental and emotional fuel needed for the difficult work of healing.
- It can take the edge off panic and severe anxiety, which is a game-changer when you're starting therapies that involve confronting traumatic memories.
By laying this groundwork, medication helps you squeeze every bit of value out of the time and effort you're putting into therapy. This teamwork is often the key to building real momentum.
SSRIs: The Go-To Medication for PTSD
The most common medications prescribed for PTSD are a type of antidepressant known as Selective Serotonin Reuptake Inhibitors (SSRIs). You've probably heard of some of them, like Zoloft and Paxil, which are the two officially approved by the FDA for treating PTSD.
SSRIs work by boosting the levels of serotonin in the brain, a natural chemical that helps regulate mood, sleep, and our overall sense of well-being. They're often very good at dialing back symptoms like depression, worry, irritability, and impulsiveness. While a psychiatrist might consider other options based on your specific needs, SSRIs are typically the first thing they'll try.
It’s crucial to see medication as a support system, not the entire solution. It manages the symptoms, but therapy does the heavy lifting of resolving the trauma itself. They're a team.
The Proof is in the Results
This integrated strategy isn't just a nice theory—it's backed by solid evidence. While trauma-focused therapies consistently post the best success rates for resolving PTSD, adding medication can give many people the extra support they need to get there.
Take a look at the data from VA healthcare systems, for example. When veterans receive trauma-focused therapies like Prolonged Exposure, 53 out of 100 achieve what's considered full remission. That's a powerful number. For those using medication alone, that number is 42 out of 100. While both are helpful, the research makes it clear that therapy is the most effective tool in the box, and a combined approach can make it even more accessible. You can read more about these treatment outcomes for PTSD.
At reVIBE Mental Health, our whole model is built around this idea. Your therapist and psychiatric provider are on the same team, collaborating on your care. This ensures your treatment plan is seamless and built just for you, giving you the comprehensive support needed for a stronger, more lasting recovery.
Finding the Right Therapist for Your PTSD Treatment

Let’s be clear about one thing: the single most important part of your recovery isn't the specific type of therapy you choose. It's the connection you feel with your therapist. Finding the right person is everything, because this relationship is the safe harbor where you'll do the hard work of healing.
But how do you even start looking? It helps to have a practical roadmap. Knowing what to look for and which questions to ask will give you the confidence to find a specialist who feels right for you.
What Credentials to Look For
As you search, you'll see a lot of acronyms after therapists' names. LPC, LCSW, PsyD… what does it all mean? While they might seem a bit confusing, these letters simply tell you about a professional's level of education, training, and licensure.
Here are a few of the most common ones you'll run into:
- LPC (Licensed Professional Counselor): These professionals have a master's degree in counseling and are trained to diagnose and treat mental health disorders.
- LCSW (Licensed Clinical Social Worker): An LCSW also holds a master's degree but often brings a "person-in-environment" perspective, looking at how your social and family systems play a role.
- PhD or PsyD: These are doctoral-level psychologists. A PhD typically has a strong background in research, while a PsyD focuses more on clinical practice.
Beyond the basics, you really want to look for specific certifications in trauma-focused therapies. Someone who is "Certified in EMDR" or "Certified in TF-CBT" has gone through demanding, advanced training in these gold-standard methods. It's proof they have the specialized skills to treat PTSD effectively. A well-rounded psychiatric mental health practitioner will often hold these kinds of specialized credentials.
Essential Questions to Ask a Potential Therapist
Finding a good fit goes way beyond credentials on a wall. It's about feeling safe, heard, and genuinely understood. Before you commit, it's a great idea to schedule a brief consultation call to ask some key questions. This initial chat can tell you a surprising amount about their style and whether you'll click.
Here’s a quick checklist to guide that first conversation:
- Experience with Trauma: "What's your experience treating PTSD, especially related to [your type of trauma, e.g., an accident, combat, sexual assault]?"
- Therapeutic Approach: "What types of therapy do you typically use for PTSD? Are you trained in specific methods like EMDR or TF-CBT?"
- Treatment Philosophy: "How do you see the relationship between therapist and client in the healing process?"
- First Few Sessions: "What can I expect in our first couple of sessions? How do we work together to set goals?"
Remember, you are interviewing them for a very important role in your life. It is perfectly okay to speak with a few different therapists before you find the one that clicks. Trust your gut instinct.
Don't forget that personal factors in choosing a therapist, like their gender or cultural background, can also make a huge difference in how comfortable you feel opening up.
What to Expect in Your First Few Sessions
Your first appointments are all about building a foundation of trust. You won't be expected to dive headfirst into the most painful parts of your trauma right away—that wouldn't be safe or effective.
Instead, the initial focus is on getting to know each other. Your therapist will want to understand your history and your symptoms, but most importantly, they will work with you to establish a sense of safety in the room. Together, you'll set some goals for what you want to get out of therapy. This early phase ensures you feel secure and ready before the deeper work begins.
How to Start Your Healing Journey in Arizona
Deciding to get help is a huge step, but figuring out how to actually do it can feel overwhelming. We get it. That's why we've made the process of finding expert, compassionate PTSD therapy in Arizona as simple and clear as possible, taking the guesswork out so you can focus on your recovery.
The first move is always the hardest, but we've made it easy: just reach out. One phone call to reVIBE Mental Health connects you with a real person on our care team. They're here to listen, answer your initial questions, and get you scheduled. No complicated hoops to jump through.
Our teams are built around the most effective, evidence-based treatments for trauma, like EMDR and Trauma-Focused CBT. We also have in-house psychiatry, which means if medication is part of your plan, your care is all under one roof—coordinated and seamless from day one.
A Simple Path to Getting Started
We believe getting started shouldn't be another source of stress. Here’s what the first few steps look like when you connect with us.
- Make the Call: The journey begins when you call us at (480) 674-9220. You’ll speak with a helpful care coordinator, not a machine.
- A Quick Chat: They'll ask a few straightforward questions to get a sense of what you're dealing with. This helps us match you with the right therapist and the right kind of care for you.
- Insurance & Scheduling: We’ll handle the insurance verification for you and find a time that fits your life, whether you prefer to come in person or meet online.
- Meet Your Therapist: Your first appointment is all about building a connection. It's a time for you to get comfortable, feel safe, and start working together to map out your goals for healing.
Our goal is simply to connect you with the right support, right away.
The most important part of this process is that you are in control. Our team is here to support you in finding a therapeutic path that feels safe, respectful, and tailored to your unique experiences and needs.
Find a reVIBE Location Near You!
You can check out all our offices and get directions on our reVIBE Mental Health locations page.
We currently have five locations for your convenience. (480) 674-9220
reVIBE Mental Health – Chandler
3377 S Price Rd, Suite 105, Chandler, AZ
reVIBE Mental Health – Phoenix Deer Valley
2222 W Pinnacle Peak Rd, Suite 220, Phoenix, AZ
reVIBE Mental Health – Phoenix PV
4646 E Greenway Road, Suite 100, Phoenix, AZ
reVIBE Mental Health – Scottsdale
8700 E Via de Ventura, Suite 280, Scottsdale, AZ
reVIBE Mental Health – Tempe
3920 S Rural Rd, Suite 112, Tempe, AZ
Your Questions About PTSD Therapy, Answered
It’s completely normal to have questions when you’re thinking about starting therapy for PTSD. Knowing what to expect can make the first step feel a lot less intimidating. Let's walk through some of the most common things people wonder about.
How Long Does Therapy for PTSD Usually Take?
There’s no magic number here—everyone’s journey is different. That said, many of the most effective, research-backed therapies are designed to be relatively short-term.
For therapies like Cognitive Processing Therapy (CPT) or Prolonged Exposure (PE), you might be looking at a course of about 12 to 15 sessions. Many people see incredible results with EMDR in a similar timeframe.
But if you’re dealing with complex or long-term trauma, your therapy might take a bit longer. The goal isn’t to hit a specific number of sessions; it’s to help you find lasting healing at a pace that feels right for you. Your therapist will work with you to figure out what that looks like.
Will I Have to Talk About My Trauma in Detail?
This is probably the biggest question—and fear—for most people, and the answer is: not necessarily. You are in control, and you have options.
- In some approaches, like Prolonged Exposure, talking through the memory in a safe and structured way is a key part of the healing process. It helps take the power out of the memory.
- But in other highly effective methods, like EMDR, you don’t have to give a detailed, play-by-play account. The focus is more on processing the internal experience—the thoughts, feelings, and body sensations connected to the memory.
A good therapist will explain the different paths you can take and help you choose the one that feels most comfortable and respectful of your experience. Your safety comes first.
Is it possible to fully recover from PTSD?
Yes, absolutely. Recovery doesn’t mean you’ll forget what happened, but it does mean the trauma no longer runs your life. The goal is to get to a place where the symptoms are gone, or so minimal they don’t get in your way, allowing you to move forward freely.
What if a Therapy Doesn’t Work for Me?
It’s okay if the first thing you try isn't the right fit. Healing isn't a one-size-fits-all experience, and what works wonders for one person might not click for another. This is perfectly normal.
A great therapist will check in with you regularly to see how things are going. If a particular approach isn’t helping, they’ll be ready to pivot, either by adjusting the technique or by exploring a different evidence-based therapy that might be a better match for you.
Honest communication is everything. It's also important to consider how PTSD can affect your physical health. For example, many people explore the intricate link between PTSD and sleep apnea, and addressing these co-occurring issues is part of a holistic recovery plan.
At reVIBE Mental Health, our compassionate team is here to answer all your questions and help you find a path forward. To learn more or schedule your first appointment, please visit us at https://revibementalhealth.com.