When you're trying to figure out if DBT or CBT is the right fit, it often boils down to this: Cognitive Behavioral Therapy (CBT) helps you change your relationship with your thoughts, while Dialectical Behavior Therapy (DBT) helps you change your relationship with your emotions.
CBT gives you the tools to identify and challenge thoughts that aren't serving you. DBT, on the other hand, equips you with the skills to both accept and manage powerful, often overwhelming feelings.
DBT vs CBT: Understanding the Core Differences
Stepping into the world of therapy can feel like learning a new language, with a whole alphabet of acronyms like CBT and DBT being thrown around. While they're both highly effective, evidence-based forms of "talk therapy," they come from different places and are built to tackle different kinds of challenges. Getting clear on what makes them unique is the best first step toward finding what you truly need.

Think of Cognitive Behavioral Therapy (CBT) as being a bit like a detective for your mind. It’s grounded in a straightforward idea: our thoughts, feelings, and actions are all connected. A negative thought pops up, which kicks off a difficult feeling, and that feeling can easily lead to an unhelpful behavior. CBT gives you a structured way to pinpoint these automatic thought patterns—what therapists call cognitive distortions—and actively question them. It's very goal-oriented and focused on solving current problems by changing how you think.
Dialectical Behavior Therapy (DBT) actually grew out of CBT. It was specifically developed to help people who feel their emotions with an overwhelming intensity that can derail their lives. DBT takes the change-focused strategies from CBT and adds a game-changing ingredient: acceptance.
The central "dialectic" in DBT is finding the balance between accepting yourself and your feelings just as they are, right now, while also committing to the work needed to build a better life.
DBT operates on the principle that two seemingly opposite things can be true at the same time: You can accept your current reality and emotional pain, and you can work to change your behaviors to create the life you want.
This dual approach is what makes DBT so powerful for managing severe emotional distress, stopping destructive behaviors, and rebuilding relationships.
Core Philosophy and Goals
At its core, CBT’s goal is to reduce symptoms by helping you identify and restructure specific negative or irrational thoughts. For instance, if you make a small mistake at work and your immediate thought is, "I'm a total failure," a CBT therapist would guide you in looking for the actual evidence and finding a more realistic, balanced perspective.
DBT's goal is much broader: it’s about helping you build a "life worth living," whatever that means for you. It does this by teaching you a set of concrete, practical skills across four main areas: mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. It's less about dismantling one specific thought and more about building a comprehensive toolkit to navigate any emotional storm that comes your way.
DBT vs CBT: A Quick Comparison
To see these distinctions side-by-side, this table breaks down the key differences between the two approaches. It’s a helpful starting point for understanding where each therapy shines.
| Feature | Cognitive Behavioral Therapy (CBT) | Dialectical Behavior Therapy (DBT) |
|---|---|---|
| Primary Focus | Changing unhelpful thought patterns to influence behavior and emotions. | Accepting intense emotions while learning skills to manage them and improve relationships. |
| Core Principle | Thoughts create feelings, and changing thoughts can change how you feel and act. | Balancing acceptance and change to build a life worth living. |
| Ideal For | Specific issues like anxiety, phobias, depression, and OCD. | Severe emotional dysregulation, self-harm, BPD, and complex trauma. |
| Key Strategy | Identifying cognitive distortions and using evidence to challenge them. | Learning skills in mindfulness, distress tolerance, and emotion regulation. |
Ultimately, CBT is a targeted approach for specific thought-driven problems, whereas DBT offers a broader, skills-based framework for those who struggle with intense, hard-to-manage emotions.
How Cognitive Behavioral Therapy Works
Cognitive Behavioral Therapy, or CBT, works from a simple but powerful idea: what you think directly affects how you feel and what you do. It’s a very practical, hands-on therapy that helps you become an expert on your own mind. The fundamental goal is to show you that by changing your thoughts, you can change your life.

At the heart of CBT is the cognitive triangle. This model shows how your thoughts, emotions, and behaviors are all linked. Think of it this way: a negative thought pops up, sparking a tough emotion, which then prompts an unhelpful action. This creates a vicious cycle that can feel impossible to escape.
Identifying Unhelpful Thought Patterns
A huge part of the CBT journey is learning to spot cognitive distortions. These are essentially glitches in our thinking—common, irrational patterns that twist our perception of reality and fuel negative feelings. A therapist at reVIBE Mental Health acts as a guide, teaching you how to become a detective of your own thoughts and catch these distortions in the act.
Here are a few common cognitive distortions you might recognize:
- All-or-Nothing Thinking: Seeing things in black and white. If your performance isn't perfect, you might see it as a complete failure.
- Catastrophizing: Your mind immediately jumps to the worst-case scenario, no matter how unlikely it actually is.
- Overgeneralization: You take one single negative event and turn it into a never-ending pattern of defeat.
- Personalization: You blame yourself for things that are completely out of your control.
Just being able to name these patterns gives you a sense of control. This awareness is the crucial first step in breaking them down. If you're interested in the basics, you can learn more about what Cognitive Behavioral Therapy is and how it’s applied to different challenges.
Challenging Thoughts and Changing Behavior
Once you can spot these thought patterns, the real work begins: challenging them. CBT gives you concrete techniques to question whether your negative thoughts are actually true. A reVIBE therapist might walk you through a thought record, where you track a situation, the automatic thoughts it triggered, the emotions you felt, and then—most importantly—work on developing a more balanced, evidence-based alternative thought.
The point of CBT isn't to plaster on a fake smile with "positive thinking." It’s about fostering realistic thinking. You learn to weigh the evidence for and against your automatic thoughts to land on a more helpful and accurate perspective.
This mental work goes hand-in-hand with changing your behavior. For instance, if you struggle with social anxiety, your therapist might help you set up a behavioral experiment. You'd start by stating a fear-based prediction (like, "If I share my idea in the meeting, everyone will think it's dumb"). Then, you test that prediction in a safe, structured way.
By collecting your own real-world data, you can directly confront your fears and often prove that the catastrophe you were expecting isn't going to happen. With practice, these new ways of thinking and acting start to feel more natural, effectively rewiring the old, unhelpful cycles that were causing you so much distress.
How Dialectical Behavior Therapy Works
While Cognitive Behavioral Therapy hones in on changing your thoughts, Dialectical Behavior Therapy (DBT) comes at the problem from a different angle. It was originally developed for people who feel emotions so intensely that it wreaks havoc on their lives, relationships, and even their sense of who they are. DBT is built on a powerful core idea: the dialectic between acceptance and change.

What does that actually mean? It means learning to accept yourself and your feelings exactly as they are right now, without judgment. At the same time, you're actively working to build healthier behaviors and create a life that feels worth living. It's a huge shift from battling your emotions to understanding and working with them.
The Four Pillars of DBT Skills
DBT is a very practical, skills-based therapy. Instead of spending all your time digging into the past, it gives you a tangible toolkit for handling the emotional challenges you face today. These skills are organized into four core modules.
- Mindfulness: This is the bedrock of DBT. It’s all about learning to stay grounded in the present, simply noticing your thoughts and feelings without getting carried away by them.
- Distress Tolerance: Think of these as your crisis-survival skills. When you’re hit with an overwhelming wave of emotional pain or anger, distress tolerance offers concrete strategies to get through it without making things worse.
- Emotion Regulation: This module helps you get a handle on your emotions. You learn what they are, why you have them, and how to dial down their intensity so they aren’t calling all the shots.
- Interpersonal Effectiveness: Healthy relationships are key to a good life. These skills teach you how to ask for what you need, say no when you have to, and manage conflict in a way that protects your self-respect.
This comprehensive structure is what makes DBT so powerful. It doesn't just patch one part of the problem; it gives you a complete framework for building emotional resilience from the ground up.
Practical Application of DBT Skills
Let’s say someone struggles with explosive anger that consistently damages their relationships. A reVIBE Mental Health therapist specializing in DBT wouldn’t just talk about why they feel angry. They’d teach specific skills. For instance, in a moment of intense rage, the therapist might walk the client through a Distress Tolerance technique like the TIPP skill (Temperature, Intense exercise, Paced breathing, Paired muscle relaxation).
The goal isn't to eliminate anger but to change your response to it. DBT gives you the power to feel an intense emotion without letting it dictate your actions, preserving your relationships and self-respect.
This hands-on, skills-first approach is especially effective for those dealing with complex trauma or severe emotional dysregulation. Research consistently backs this up. In fact, one study showed that DBT significantly boosted emotion-focused coping strategies in patients recovering from a heart attack—a period of extreme stress—outperforming other therapies in that area. You can explore the full findings on DBT's impact on emotion regulation.
By giving people real tools for managing crises and navigating their feelings, DBT helps them build a life they genuinely want to live.
Diving Into the Session: What DBT vs. CBT Actually Looks Like
When you're trying to choose a therapy, understanding what actually happens in the room (or on the screen) is crucial. It’s about more than just theory; it’s about finding a structure and rhythm that fits your life and your needs. While both CBT and DBT fall under the umbrella of "talk therapy," their day-to-day practice can feel worlds apart.
CBT is laser-focused and goal-oriented. Think of it as a strategic partnership where you and your therapist are a team with a clear mission. In contrast, DBT is a much more comprehensive program, almost like an ecosystem of support, built to help people navigate really intense emotional waters.
The Focused Nature of a CBT Session
A typical CBT session is built for efficiency and runs like a well-oiled machine, usually lasting about 50 minutes. The whole point is to send you out the door with concrete tools you can use immediately, so the time is incredibly focused.
This structure gives CBT a predictable and reassuring rhythm:
- Check-in and Agenda Setting: You'll start by touching base on your week, then you and your therapist will map out what you want to accomplish in that session. This isn't just a casual chat; it's about making every minute count.
- Homework Review: In CBT, the real work often happens between sessions. You’ll go over the "homework" you were assigned—maybe a thought record or a behavioral experiment—and dig into what you discovered.
- Skill Building and Problem-Solving: This is the heart of the session. You’ll spend the bulk of your time learning a new cognitive or behavioral skill and figuring out exactly how to apply it to a specific problem you're facing.
- New Homework and Feedback: Before you leave, you'll get a new assignment to practice and have a chance to give your therapist feedback, ensuring the process is working for you.
Because it's so targeted, a full course of CBT is often designed to be short-term, typically wrapping up in about 12 to 20 weeks. It’s all about getting you to your goals efficiently.
The Comprehensive DBT Program Structure
DBT isn't just a once-a-week appointment; it's a multi-layered program designed to provide wraparound support. This is why it’s so powerful for people who feel like their emotions are constantly derailing them. A standard DBT program is built on several pillars.
Individual Therapy: This is your weekly one-on-one meeting with your therapist. The focus here is intensely practical: how to take the skills you're learning and apply them to the messy reality of your life. You’ll also work on staying motivated and tackling anything that gets in the way of your progress.
Group Skills Training: This is a core part of the program, but it feels more like a class than a typical therapy group. Each week, you’ll learn and practice very specific skills from the four DBT modules: mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness.
Phone Coaching: This is a game-changer. DBT provides a lifeline between sessions. You can call your therapist for quick, in-the-moment coaching to help you use your skills when a crisis hits, rather than waiting a whole week to talk about it.
This multi-pronged approach is what makes DBT so effective. It ensures that you're not just learning skills in a vacuum but are actively supported in using them when life gets difficult.
Given its depth, a full DBT program is a real commitment. You can expect it to last anywhere from six months to a year, giving you the time needed to truly internalize and master a whole new way of living.
Therapy Structure and Format DBT vs CBT
To give you a clearer picture, this table breaks down the fundamental structural differences between how a typical course of CBT and DBT is set up.
| Aspect | Cognitive Behavioral Therapy (CBT) | Dialectical Behavior Therapy (DBT) |
|---|---|---|
| Session Format | Primarily individual therapy sessions. | A combination of individual therapy, group skills training, and phone coaching. |
| Typical Duration | A shorter-term therapy, often 12-20 weekly sessions. | A longer-term program, typically lasting 6 months to one year. |
| In-Session Focus | Structured agenda, reviewing homework, learning and applying specific cognitive techniques. | Applying skills to life events, problem-solving, and managing therapy progress. |
| Between Sessions | Practice-based "homework" like thought records or behavioral experiments. | Applying learned skills, with the option for as-needed phone coaching for real-time support. |
| Therapeutic Relationship | Collaborative and educational, with the therapist acting as a coach or guide. | A validating and supportive partnership that balances acceptance with a push for change. |
Ultimately, the right structure depends entirely on what you're trying to achieve. CBT’s direct, time-limited approach is fantastic for specific issues, while DBT’s immersive, multi-component program offers the deep, consistent support needed for more complex emotional challenges.
Which Conditions Each Therapy Treats Best
Figuring out whether DBT or CBT is the right fit often boils down to what you're struggling with. While they're both powerful, they were designed to tackle different kinds of problems. It’s a bit like choosing between a specialist and a general practitioner—each has a unique skill set for certain conditions.
CBT is widely seen as the gold standard for many common mental health issues. Its logical, structured nature is incredibly effective when specific, unhelpful thought patterns are the main source of distress.
When CBT Is the Front-Runner
CBT really shines when the mission is to pinpoint, question, and ultimately change destructive thinking habits. This targeted strategy makes it a great choice for several conditions.
- Anxiety Disorders: For things like panic disorder, generalized anxiety, and phobias, CBT gives you a framework to confront the "worst-case scenario" thoughts that fuel fear. Our guide on the types of therapy for anxiety dives deeper into how this works.
- Depression: CBT offers practical tools to push back against the negative self-talk and hopelessness that drain your energy, helping you slowly rebuild healthier daily routines.
- Obsessive-Compulsive Disorder (OCD): A specialized form of CBT known as Exposure and Response Prevention (ERP) is the number one treatment for OCD. It directly helps people break the exhausting cycle of obsessions and compulsions.
In these situations, the work is all about rewiring the cognitive "software" that keeps the symptoms running.
Where DBT Shines Brightest
Dialectical Behavior Therapy, on the other hand, was built from the ground up to help with intense, overwhelming emotional dysregulation. It gets to the heart of the emotional pain that can make life feel impossible and lead to harmful behaviors.
DBT is the go-to treatment for:
- Borderline Personality Disorder (BPD): It was the first therapy proven to work for BPD, and it continues to be the most researched and successful treatment we have.
- Chronic Suicidal Thoughts and Self-Harm: The skills taught in DBT, especially distress tolerance, offer real, in-the-moment alternatives when destructive urges feel overpowering.
- Complex PTSD (C-PTSD): For anyone who has endured long-term trauma, DBT helps manage the intense emotional flashbacks and relationship struggles that often follow, rebuilding a much-needed sense of safety.
DBT’s true power is helping people who feel like their emotions are completely out of control. It teaches you how to ride the waves of intense feeling instead of being drowned by them, creating a path toward stability and a life you actually want to live.
This focus on managing big emotions and accepting reality makes it a perfect fit for these complex challenges.
The Overlap: Conditions Like Eating Disorders
Sometimes, the choice isn't so black and white. For certain conditions, like eating disorders, both therapies can be effective, and the best one often depends on what’s driving the behavior.
If the eating disorder is fueled by distorted thoughts about body image and food (like, "If I eat that, I'm a failure"), CBT's focus on challenging those beliefs is a direct hit. But if the behaviors are a way to cope with overwhelming feelings of shame or anxiety, DBT’s skills for emotion regulation might be more useful.
The research shows just how nuanced this can be. A 2022 study on Binge Eating Disorder found that an enhanced CBT approach worked better right after treatment ended. However, at the 6-month follow-up, DBT was just as effective—and it took half the therapy time. This shows how both therapies can create lasting change, just through different doors. Learn more about the study's findings on eating disorder treatments.
Ultimately, a skilled therapist at a place like reVIBE Mental Health can help you figure out which approach, or even a blend of both, will best address your unique situation and help you heal.
How to Choose the Right Therapy for You
Picking between DBT and CBT isn’t about finding the "best" therapy—it's about matching the right tool to your specific needs. When you strip away the clinical jargon, the choice often boils down to one simple question: Are you trying to change what you think, or are you trying to manage how you feel? Answering that honestly is your first step toward finding a path that genuinely works.
This decision tree helps visualize that core distinction. It guides you toward either the thought-focused approach of CBT or the emotion-focused framework of DBT, depending on what you want to achieve.
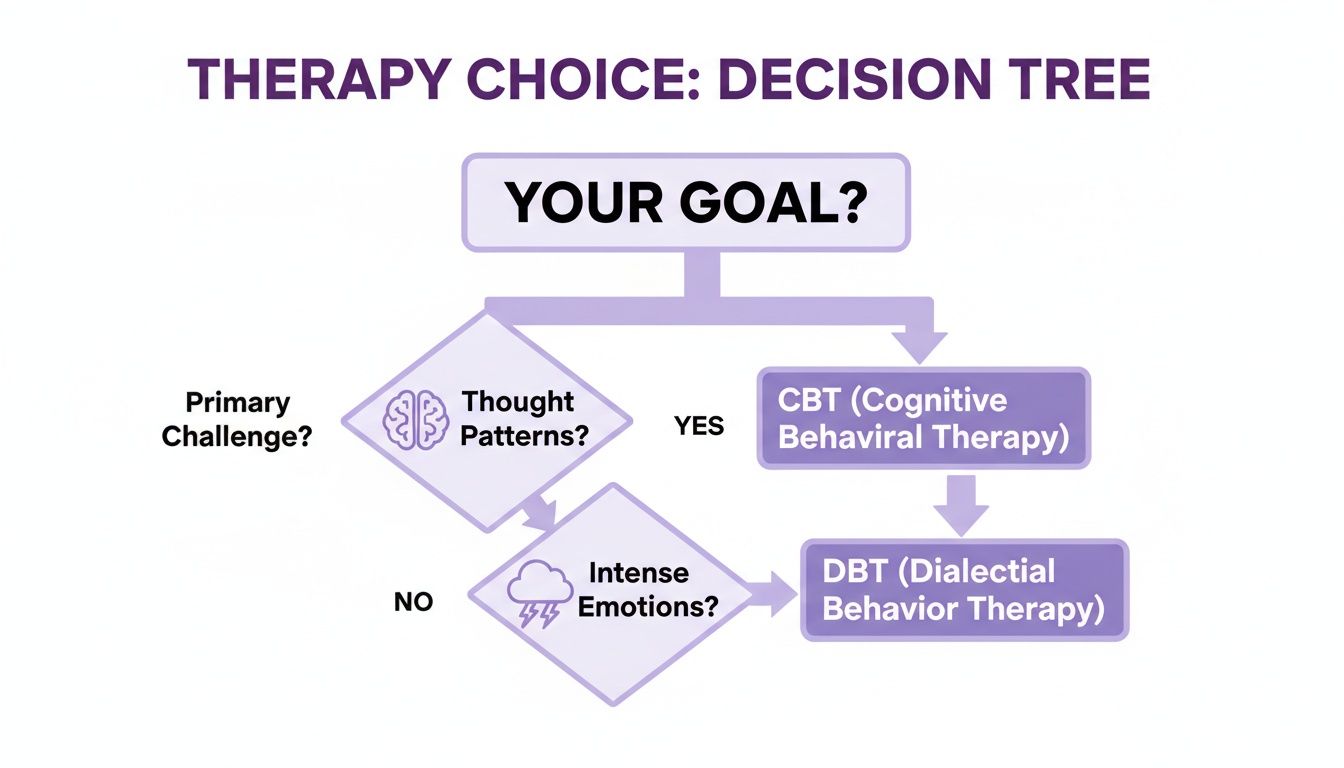
The image breaks it down cleanly: if your biggest battle is with specific, repeating thought patterns, CBT is often the most direct path forward. But if overwhelming emotions are derailing your life, DBT gives you the practical toolkit you need to regain control.
Aligning Your Goals with the Right Approach
To feel confident in your decision, it helps to start with a little self-reflection. The trick is to get clear on the main source of your distress.
Think about these real-world examples:
Scenario 1: The CBT Path. Let's say your goal is to silence the negative self-talk that’s fueling your anxiety at work. You find yourself constantly worrying about making a mistake and assuming your boss is disappointed, even when there's no proof. In this situation, CBT’s practical, thought-focused tools are a perfect fit. A therapist would work with you to pinpoint and challenge those cognitive distortions head-on.
Scenario 2: The DBT Path. Now imagine your goal is to build emotional resilience and stop destructive patterns in your relationships. You experience intense mood swings that lead to explosive arguments, and you often feel swamped by shame or anger afterward. Here, DBT's skills-based, holistic framework is going to be far more effective. It’s designed to teach you how to sit with distress and regulate your emotions so they no longer run the show.
Considering the Nuances in Effectiveness
Both therapies are well-proven when it comes to boosting psychological resilience, but recent studies have started to uncover some subtle yet important differences. While both work, some research suggests DBT might have a slight edge in fostering certain aspects of mental strength.
For instance, a 2024 study found that while both DBT and Group CBT (GCBT) were effective, DBT showed a small but significant advantage in enhancing optimism, hope, and overall psychological capital. Some of the effect sizes reached up to 0.667, which is noteworthy. This hints that for people who aren't just trying to reduce symptoms but actively want to build a more hopeful and resilient outlook, DBT might offer a bit more.
Your choice is deeply personal. Are you looking for a structured, targeted intervention for specific thoughts (CBT)? Or do you need a broader, skills-based program to manage intense emotional experiences (DBT)?
Ultimately, when weighing DBT against CBT, looking at factors like patient satisfaction can also offer clues about which therapy aligns with what you expect to get out of the experience. Your journey is your own, and choosing the right approach is a powerful first move toward feeling better.
Finding a DBT or CBT Therapist in Arizona
Deciding to start therapy is a huge step, and finding the right person to guide you shouldn't feel like another mountain to climb. Whether you’ve read through this guide and are leaning toward CBT’s practical structure or DBT’s focus on emotional skills, the most important thing is finding a professional who truly gets it. At reVIBE Mental Health, our whole focus is on making that connection feel as straightforward and supportive as possible.
The process is simple. It all starts with a confidential call or a quick online message. Our first priority is to listen to what’s going on and carefully match you with a therapist whose expertise fits your unique situation—whether that’s in DBT, CBT, or another evidence-based approach. We know you’re not a diagnosis; you’re a person, and your care should reflect that.
Find a reVIBE Location Near You!
We currently have five locations for your convenience. (480) 674-9220
reVIBE Mental Health – Chandler
3377 S Price Rd, Suite 105, Chandler, AZ
reVIBE Mental Health – Phoenix Deer Valley
2222 W Pinnacle Peak Rd, Suite 220, Phoenix, AZ
reVIBE Mental Health – Phoenix PV
4646 E Greenway Road, Suite 100, Phoenix, AZ
reVIBE Mental Health – Scottsdale
8700 E Via de Ventura, Suite 280, Scottsdale, AZ
reVIBE Mental Health – Tempe
3920 S Rural Rd, Suite 112, Tempe, AZ
Your First Steps with reVIBE Mental Health
Walking into therapy for the first time can be nerve-wracking. We’ve designed our entire process to be as clear and reassuring as possible, creating a space where you feel safe and understood right from the first hello.
At the end of the day, the DBT vs. CBT debate comes down to one thing: finding a skilled professional who can accurately assess your symptoms and work with you to build a treatment plan. The therapeutic relationship is the bedrock of real, lasting change.
We also do our best to take the logistical headaches out of the equation. We accept most major insurance plans and can help you figure out your coverage so there are no surprises. Life is busy, so we offer flexible scheduling with options for both in-person sessions and secure online appointments. This same flexibility is transforming how care is delivered; for practitioners, the rise of remote psychiatry jobs is making it possible to connect with more people than ever before.
Our team works collaboratively to ensure you get a truly comprehensive care plan. You can get to know our dedicated professionals and find a therapist at reVIBE Mental Health who is ready to partner with you. Whether you’re looking for short-term coping skills or longer-term therapy, we’re here to help you rediscover your strength and start feeling better.
Ready to take the next step? The team at reVIBE Mental Health is here to provide the compassionate, expert care you deserve. Visit us online to get started or call (480) 674-9220 today.